 Figure 8-31 Pityriasis rosea.
A herald patch is present on the breast. Subsequent lesions commonly begin in
the lower abdominal region.
Figure 8-31 Pityriasis rosea.
A herald patch is present on the breast. Subsequent lesions commonly begin in
the lower abdominal region.
Pityriasis rosea is a common, benign, usually asymptomatic, distinctive, self-limiting skin eruption of unknown etiology. [125] There is some evidence that it is viral in origin. Small epidemics have occurred in fraternity houses and military bases. It is predominant among women by a margin of 1.5 to 1. More than 75% of patients are between the ages of 10 and 35 years, with a mean age of 23 years and an age range of 4 months to 78 years. Two percent of patients have a recurrence. [126] The incidence of disease is higher during the colder months. Twenty percent of patients have a recent history of acute infection with fatigue, headache, sore throat, lymphadenitis, and fever; the disease may be more common in atopic patients. Pityriasis rosea has several unique features, but variant patterns do exist; these may create confusion between pityriasis rosea and secondary syphilis, guttate psoriasis, viral exanthems, tinea, nummular eczema, and drug eruptions.
Typically, a single 2- to 10-cm round-to-oval lesion, the herald patch, abruptly appears. It may occur anywhere on the body, but is most frequently located on the trunk or proximal extremities. The herald patch retains the same features as the subsequent oval lesions. At this stage, many patients are convinced that they have ringworm.
Within a few days to several weeks (average 7 to 14 days) the disease enters the eruptive phase. Smaller lesions appear and reach their maximum number in 1 to 2 weeks ( Figure 8-31 ). They are typically limited to the trunk and proximal extremities, but in extensive cases they develop on the arms, legs, and face (Figure 8-32) . Lesions are typically benign and are concentrated in the lower abdominal area ( Figure 8-33 ). Individual lesions are salmon pink in whites and hyperpigmented in blacks. Many of the earliest lesions are papular, but in most cases the typical 1- to 2-cm oval plaques appear (Figure 8-34) . A fine, wrinkled, tissuelike scale remains attached within the border of the plaque giving the characteristic ring of scale, called collarette scale ( Figure 8-35 ). The long axis of the oval plaques is oriented along skin lines. Numerous lesions on the back, oriented along skin lines, give the appearance of drooping pine-tree branches, which explains the designation Christmas-tree distribution. The number of lesions varies from a few to hundreds. In rare instances the lesions seem to cover the entire skin surface. A variety of oral lesions has been reported. [127] [128]
 Figure 8-31 Pityriasis rosea.
A herald patch is present on the breast. Subsequent lesions commonly begin in
the lower abdominal region.
Figure 8-31 Pityriasis rosea.
A herald patch is present on the breast. Subsequent lesions commonly begin in
the lower abdominal region.
 Figure 8-32 Pityriasis rosea.
The fully evolved eruption 2 weeks after onset.
Figure 8-32 Pityriasis rosea.
The fully evolved eruption 2 weeks after onset.
 Figure 8-33 Pityriasis rosea.
Lesions are typically concentrated in the lower abdominal area.
Figure 8-33 Pityriasis rosea.
Lesions are typically concentrated in the lower abdominal area.
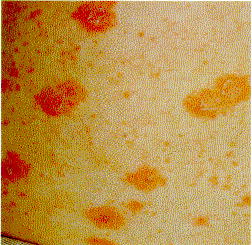 Figure 8-34 Pityriasis rosea.
Both small, oval plaques and multiple, small papules are present. Occasionally
the eruption consists only of small papules.
Figure 8-34 Pityriasis rosea.
Both small, oval plaques and multiple, small papules are present. Occasionally
the eruption consists only of small papules.
 Figure 8-35 Pityriasis rosea.
A ring of tissuelike scale (collarette scale) remains attached within the border
of the plaque.
Figure 8-35 Pityriasis rosea.
A ring of tissuelike scale (collarette scale) remains attached within the border
of the plaque.
In some cases other types of lesions predominate. The papular variety is more common in young children, pregnant women, and blacks (Figures 8-36 and 8-37) . Vesicular and, rarely, purpuric [129] lesions are seen in infants and children.
Most lesions are asymptomatic, but many patients complain of mild transient itching. Severe itching may accompany extensive inflammatory eruptions. The disease clears spontaneously in 1 to 3 months. There may be postinflammatory hyperpigmentation, especially in blacks.
The experienced observer can rely on a clinical impression to make the diagnosis. Tinea can be ruled out with a potassium hydroxide examination. Secondary syphilis may be indistinguishable from pityriasis rosea, especially if the herald patch is absent. A serologic test for syphilis should be ordered if a clinical diagnosis cannot be made. [130] A biopsy is useful in atypical cases; it reveals extravasated erythrocytes within dermal papillae and dyskeratotic cells within the dermis. Pityriasis rosea may also be mimicked by psoriasis and nummular eczema.
Whether or not PR is contagious is unknown. The disease is benign and self-limited and does not appear to affect the fetus; therefore, isolation is unnecessary. Group V topical steroids and oral antihistamines may be used as needed for itching. The rare extensive case with intense itching responds to a 1- to 2-week course of prednisone (20 mg twice a day). Direct sun exposure hastens the resolution of individual lesions, whereas those in protected areas, such as under bathing suits, remain (see Figure 8-31) . Ultraviolet light B (UVB), administered in five consecutive daily erythemogenic exposures, results in decreased pruritus and hastens the involution of lesions. Therapy is most beneficial within the first week of the eruption. [131]
 Figure 8-37 Pityriasis rosea.
Papular lesions are seen in children,
Figure 8-37 Pityriasis rosea.
Papular lesions are seen in children,
pregnant women, and
blacks.